Blogs
Zygomatic Dental Implants in Antalya

Table of Contents
For many patients, tooth loss is not just a physical problem it also brings uncertainty and emotional stress. This is especially true for people who have been told they are not suitable candidates for traditional dental implants due to severe bone loss in the upper jaw. Hearing “there is no solution” can be discouraging and confusing.
This article is not written to promote a treatment, but to answer the real questions patients ask when they are searching for clarity. From concerns about pain and safety to recovery time and long-term results, each section is designed to provide clear, honest, and patient-focused information.
The goal is to help you understand your options in a calm and transparent way, without medical jargon or pressure, so you can make an informed decision that feels right for you.
What are zygomatic implants and how are they different from regular implants?
Many patients first come across this treatment option after being told that standard dental implants are not possible for them. The main reason is usually severe bone loss in the upper jaw, which makes it difficult for conventional implants to stay stable.
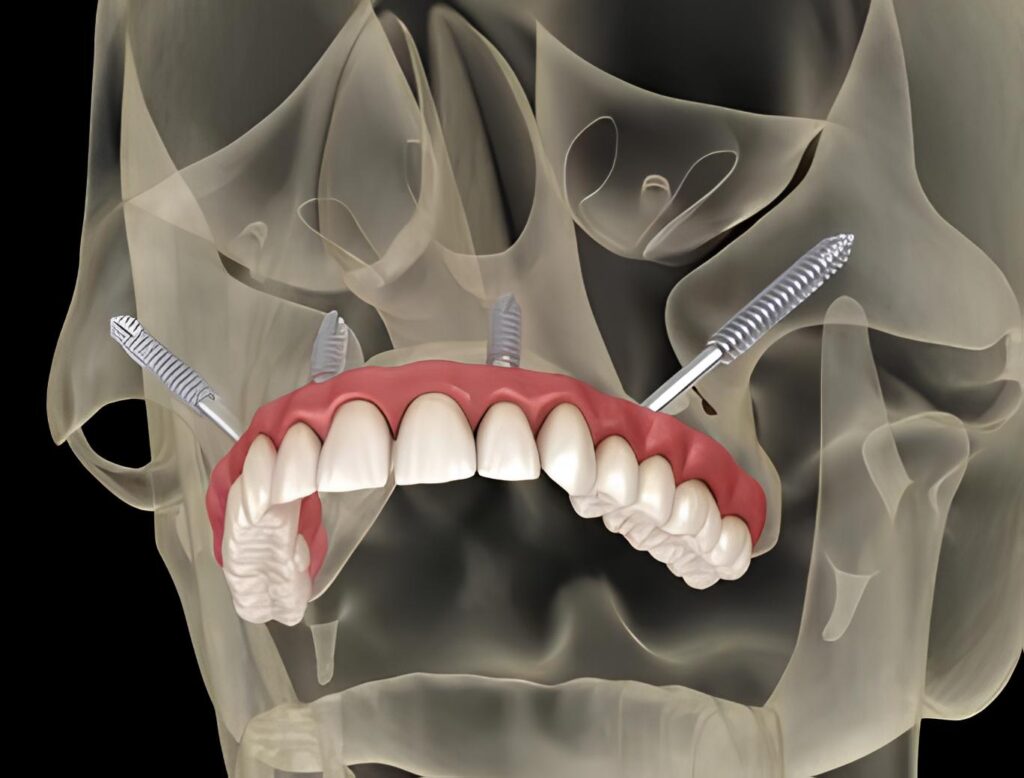
Zygomatic dental implants are different because they are anchored in the zygoma bone (cheekbone) instead of the upper jawbone. This bone is naturally stronger and denser, which allows the implant to be placed securely even when there is not enough bone in the jaw.
Another key difference is implant length. These implants are longer than regular ones and follow a different angle to reach the cheekbone safely. Because of this approach, patients often do not need bone grafting or sinus lift procedures, which can shorten the overall treatment time.
From a patient’s perspective, the biggest distinction is not just technical it’s practical. This method offers a solution for people who were previously told they had “no option,” helping them regain chewing function, stability, and confidence without going through multiple complex procedures.
Who is considered a good candidate for this treatment?
This question usually comes from patients who have already been turned down for traditional implants. If you have been told that there is not enough bone in your upper jaw, you are not alone and this is often the starting point for considering alternative solutions.
This treatment is generally suitable for patients with advanced bone loss in the upper jaw, especially those who cannot undergo bone grafting or sinus lift procedures for medical or personal reasons. It is also an option for people who have been wearing removable dentures for many years and are looking for a more stable, fixed solution.
Age alone is not a limiting factor. What matters more is overall health, bone quality in the cheekbone area, and the ability to heal properly after surgery. Patients with controlled chronic conditions can often still be evaluated for this approach after a detailed medical assessment.
Most importantly, this option is considered when traditional implant methods are no longer viable. For many patients, it represents a second chance offering stability, comfort, and the possibility of fixed teeth when they believed it was no longer achievable.
Can this treatment be done if I have severe bone loss in my upper jaw?
For many patients, severe bone loss in the upper jaw is the main reason they are told implant treatment is not possible. This situation often develops after years of tooth loss, long-term denture use, or advanced gum disease. Hearing that there is “not enough bone” can feel like the end of the road.
In cases like this, this treatment approach is specifically considered because it does not rely on the weakened upper jawbone for support. Instead, the implant is stabilized in a stronger bone structure, which allows treatment to move forward even when bone loss is advanced.
From a patient’s point of view, this means something very important: the lack of bone in the upper jaw does not automatically eliminate the possibility of fixed teeth. In many situations, patients who were previously not eligible for implants can still be evaluated for this option after proper imaging and examination.
Every case is different, and a detailed assessment is essential. However, severe bone loss alone is often not a barrier anymore it is simply a factor that guides the treatment plan toward a more suitable solution.
Is bone grafting or sinus lift required for this treatment?
One of the biggest concerns patients have is the idea of additional surgical procedures. Bone grafting and sinus lift treatments are often described as long, uncomfortable, and requiring extended healing periods. Many patients look for alternatives specifically to avoid these steps.
In most cases, this treatment does not require bone grafting or a sinus lift. Because the implants are supported by a stronger bone structure rather than the upper jawbone, the need to rebuild lost bone is usually eliminated. This is one of the main reasons the approach is recommended for patients with advanced bone loss.
For patients, this often means a shorter overall treatment timeline and fewer surgical stages. Instead of waiting months for grafted bone to heal, treatment planning can move forward more directly, depending on individual conditions.
That said, every mouth is unique. A thorough examination and imaging are essential to determine whether additional procedures are needed. Still, many patients are relieved to learn that extensive bone augmentation is often not part of this process.
Our YouTube Videos
How is the surgical procedure performed step by step?
For many patients, the word “surgery” alone can cause anxiety mostly because they don’t know what to expect. Understanding the steps beforehand often helps reduce fear and build trust in the process.
The procedure usually begins with detailed planning. Advanced imaging is used to evaluate bone structure and determine the safest placement path. This preparation stage is critical and helps ensure accuracy and safety during the operation.
On the day of the procedure, treatment is performed under appropriate anesthesia so the patient remains comfortable throughout. The implants are carefully placed following the planned angle and depth. In many cases, this is done in a single surgical session rather than multiple appointments.
After placement, temporary teeth may be attached depending on the individual case. This allows many patients to leave the clinic without feeling “toothless,” which is a major emotional relief. Once the procedure is complete, patients are monitored and given clear post-operative instructions to support healing.
From a patient’s perspective, the process is often more structured and controlled than expected. Knowing each step in advance helps transform uncertainty into confidence.
Will I feel pain during or after the surgery?
Pain is one of the first concerns patients think about when considering any surgical dental procedure. Many people imagine severe discomfort, but the reality is often very different from what they expect.
During the surgery, patients do not feel pain because appropriate anesthesia is used. The goal is to keep you comfortable and relaxed throughout the entire procedure. Most patients report that they are surprised by how calm the experience feels once it begins.
After the surgery, some level of swelling or mild discomfort is normal, especially in the first few days. This is a natural part of the healing process and is usually manageable with prescribed medication and proper aftercare. For many patients, the discomfort is comparable to or even less than what they experienced with previous dental treatments.
What often reassures patients the most is that pain tends to be temporary, while the benefits of stable, fixed teeth are long-term. With clear post-operative instructions and follow-up care, most people recover more smoothly than they initially feared.
How long does the recovery and healing process take?
Recovery time is an important concern for patients, especially those who want to return to their daily routine as soon as possible. While everyone heals at a different pace, most patients find the recovery process more manageable than they expected.
In the first few days after the procedure, mild swelling and tenderness are common. This initial phase usually improves noticeably within a week. During this time, rest, proper oral hygiene, and following post-treatment instructions play a key role in comfort and healing.
The deeper healing process where the implants fully integrate with the bone takes longer and happens gradually over several months. However, this does not mean patients must pause their lives. Many people are able to resume normal activities relatively quickly, with only minor adjustments during the early stages.
From a patient’s perspective, recovery is often described as a steady improvement rather than a difficult period. Knowing what to expect and having ongoing professional support makes the healing journey feel more controlled and less stressful.
When can I start eating normally after the treatment?
Eating comfortably is a major concern for many patients, especially after a surgical procedure. The good news is that the transition back to normal eating is usually gradual and manageable when proper guidance is followed.
In the first days after treatment, a soft-food diet is generally recommended. This helps protect the surgical area and supports early healing. Foods that are easy to chew and not too hot allow patients to eat without discomfort while giving the tissues time to recover.
As healing progresses, most patients can slowly reintroduce firmer foods. This phase is typically guided by how comfortable you feel rather than a fixed timeline. Many people notice that their chewing ability improves steadily, which boosts confidence with each step.
From a patient’s point of view, the key is patience. Rushing the process is not necessary, and following dietary recommendations closely often leads to a smoother and more comfortable return to normal eating habits.
How long do zygomatic implants last? Are they permanent?
When considering any implant treatment, patients naturally want to know whether the results will last. No one wants to go through a complex procedure only to face the same problem again a few years later.
This treatment is designed as a long-term, often permanent solution. Because the implants are anchored in a strong and dense bone structure, they tend to provide excellent stability over time. With proper placement, good oral hygiene, and regular check-ups, many patients use them successfully for decades.
Longevity also depends on daily habits. Maintaining good oral care, avoiding smoking, and following professional advice all play an important role in preserving the results. Patients who take care of their oral health usually experience fewer complications and more predictable outcomes.
From a patient’s perspective, knowing that this option is built for durability brings peace of mind. It allows people to focus on living comfortably eating, speaking, and smiling without constantly worrying about their teeth.
What are the possible risks or complications I should know about?
Every medical or dental procedure comes with certain risks, and patients deserve to be informed in an open and honest way. Understanding potential complications helps set realistic expectations and allows you to make decisions with confidence rather than fear.
As with any surgical treatment, temporary swelling, bruising, or discomfort can occur in the early healing phase. These effects are usually short-lived and tend to improve steadily with proper care and follow-up. In rare cases, infection or delayed healing may occur, which is why close monitoring and good oral hygiene are essential.
Because this procedure involves a more complex anatomical area, experience and careful planning are especially important. When performed by a qualified and experienced team, the risk of serious complications is significantly reduced. This is why detailed imaging, precise technique, and post-operative guidance play such a critical role.
From a patient’s perspective, it is reassuring to know that potential risks are well understood and manageable. Open communication and regular check-ups help ensure that any concerns are addressed early and effectively.
What is the success rate of this treatment?
Patients often want clear reassurance before committing to a complex procedure. Knowing how successful a treatment is in the long term plays a major role in feeling confident about the decision.
Clinical studies and long-term follow-ups show that this approach has a high success rate, especially when performed on properly selected patients and planned carefully. The strength of the supporting bone and precise placement contribute significantly to stability and durability over time.
From a patient’s point of view, success is not just about numbers. It means being able to chew comfortably, speak clearly, and live daily life without constant worry about dentures or loose teeth. Many patients report a noticeable improvement in comfort and quality of life after treatment.
It is important to remember that success also depends on ongoing care. Regular dental visits, good oral hygiene, and following professional recommendations all help maintain positive outcomes for years to come.
Will the final result look natural and aesthetic?
Many patients worry that implant-supported teeth might look artificial or feel different from natural teeth. This concern is completely understandable especially for those who have worn removable dentures or experienced visible dental problems in the past.
The final restorations are designed to match the natural shape, color, and proportion of your face and smile. The goal is not just function, but harmony. When planned carefully, the teeth are positioned to support facial features and restore a balanced, natural appearance rather than a “fixed” or unnatural look.
From a patient’s perspective, one of the most noticeable changes is confidence. Being able to smile, laugh, and speak without worrying about how the teeth look can have a powerful emotional impact. Many people say the result feels like getting their own teeth back not something foreign or artificial.
Aesthetic success depends on individualized planning and communication. When expectations are discussed clearly and the treatment is tailored to the patient, the final outcome is usually both natural-looking and satisfying.
Is this treatment suitable for older patients?
Many older patients hesitate to explore implant options because they believe age alone may prevent them from receiving treatment. This concern is very common, but in most cases, age by itself is not a deciding factor.
What matters more than chronological age is overall health. Patients who are in generally good condition and able to heal properly can often be considered for this treatment, even at an advanced age. A thorough medical evaluation helps determine whether the body can handle the procedure safely.
From an older patient’s perspective, the motivation is often comfort and independence. Being able to eat properly, speak clearly, and avoid removable dentures can significantly improve daily life. For many, this treatment represents not just a dental solution, but a meaningful improvement in quality of life.
With careful planning and appropriate follow-up care, older patients frequently achieve stable and satisfying results. Feeling comfortable and confident again is not limited by age it is guided by the right treatment approach.
Our Google Reviews
Frequently Asked Questions
How long does the procedure take?
The surgical procedure is usually completed in a single session. The exact duration depends on the individual case, but it is often shorter than patients expect.
Will I need to stay in the hospital after the surgery?
In most cases, a hospital stay is not required. Patients are typically able to return to their accommodation on the same day after medical observation.
Can I have temporary teeth on the same day?
Yes, many patients can receive temporary fixed teeth shortly after the procedure, allowing them to leave without removable dentures.
Is this treatment safe in the long term?
When properly planned and performed by an experienced team, this treatment has a high long-term success rate and is considered a reliable solution.
How do I know if this option is right for me?
A detailed examination and imaging are essential to determine suitability. Each patient’s condition is unique, and treatment planning is always personalized.